
I have Endometriosis, I underwent surgical treatments and the disease returned. What are my options?
Recurrence of Endometriosis
Endometriosis recurrence has been defined as:
- Recurrence of pain (dysmenorrhea, dyspareunia, or pelvic pain).
- As clinical (pelvic fibrotic areas or tender nodules) or radiological detection of recurrent endometriosis lesions.
- Surgically confirmed lesions or as repeat rise of the marker CA-125 after surgery.
Recently, recurrence was defined as lesion recurrence on reoperation or imaging after previous complete excision of the disease, with 4 subtypes:
- Symptom based suspected recurrence: Symptom recurrence based on patient history, but not proven/confirmed by imaging and/or surgery.
- Imaging based suspected recurrence: Endometriosis recurrence based on imaging in patients with or without symptoms.
- Laparoscopically proven recurrence: Recurrence of visual endometriosis without histological proof: during laparoscopy endometriosis is visually observed but either not biopsied or biopsied without histologically proven endometriosis.
- Histologically proven recurrence: Recurrence of histologically proven endometriosis during laparoscopy endometriosis is visually observed and confirmed histologically.
Endometriosis recurrence rates vary widely in the literature, ranging from 0% to 89.6%. Risk factors for recurrence include surgery-associated variables (presence and extent of adhesions, radicality of surgery) and patient-related factors (positive family history, lower age at surgery).

Is there a role for secondary prevention of recurrence of disease and painful symptoms in patients treated for endometriosis?
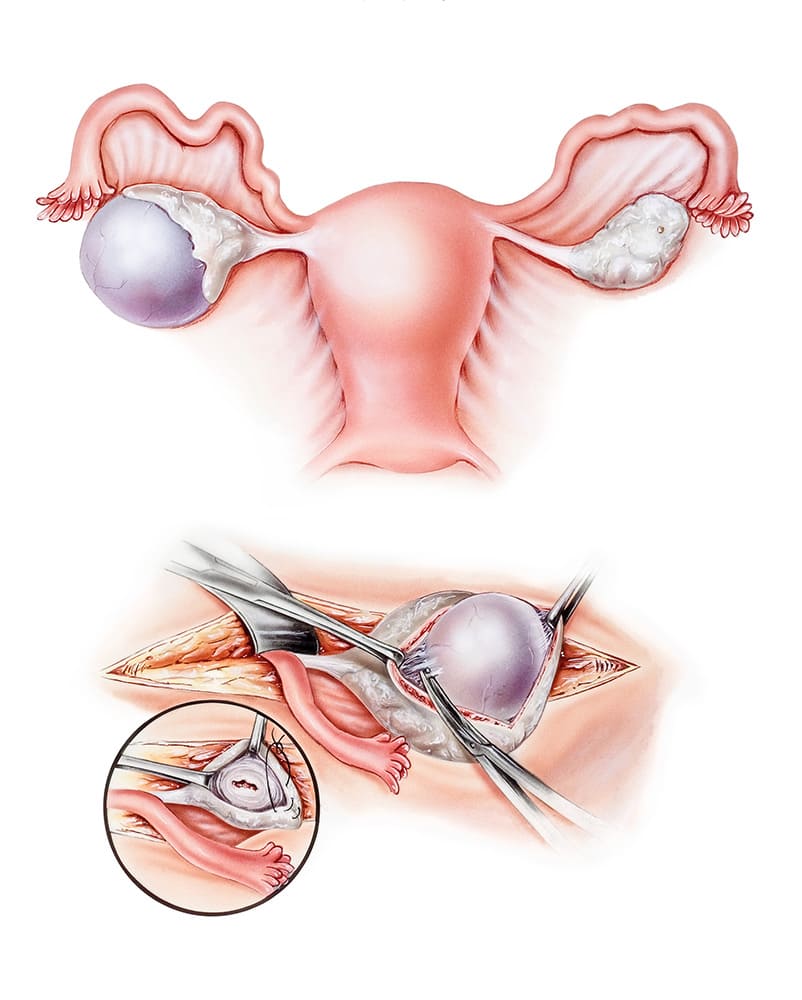
Surgical technique for prevention of recurrence in women operated on for an endometrioma (≥3 cm), clinicians should perform ovarian cystectomy, instead of drainage and electrocoagulation, for the secondary prevention of endometriosis-associated dysmenorrhea, dyspareunia, and non-menstrual pelvic pain.
Recommendation: When surgery is indicated in women with an endometrioma, clinicians should perform ovarian cystectomy, instead of drainage and electrocoagulation, for the secondary prevention of endometriosis-associated dysmenorrhea, dyspareunia, and nonmenstrual pelvic pain. However, the risk of reduced ovarian reserve should be taken into account.
Cystectomy
Is probably superior to drainage and coagulation in women with ovarian endometrioma (≥3 cm) with regard to the recurrence of endometriosis-associated pain and the recurrence of endometrioma.
A strong recommendation was formulated in favor of cystectomy. Whenever ovarian surgery is performed, the impact on ovarian reserve (i.e., the risk) should be carefully considered against the benefit.
Medical therapies for prevention of recurrence
Hormone treatment after surgery aimed at secondary prevention should be distinguished from adjunctive short-term (< 6 months) hormone treatment after surgery aimed at improving the immediate outcomes of surgery. With regard to disease recurrence, the review showed that there may be a reduction of disease recurrence in favor of postsurgical hormone therapy (OCP, GnRH agonists, danazol).
After surgical management of ovarian endometrioma in women not immediately seeking conception.
Clinicians are recommended to offer long-term hormone treatment (e.g. combined hormonal contraceptives) for the secondary prevention of endometrioma and endometriosis-associated related symptom recurrence. For the prevention of recurrence of deep endometriosis and associated symptoms, longterm administration of postoperative hormone treatment can be considered.
Factors affecting the recurrence of endometriosis following surgery. There are three main factors that can increase the risk of recurring endometriosis:
- The severity of the disease at the time of surgery: the more severe the disease, the more likely it seems to come back.
- The completeness of lesion removal: if some lesions are left behind during surgery, they may regrow with time.
- The use of medical suppressive therapy following surgery: usually reduces the recurrence of pain symptoms of endometriosis.
Symptoms of recurring endometriosis
Although many patients report symptom relief following endometriosis surgery, there is no guarantee that surgery will treat the symptoms of endometriosis.
The healing process following surgery
The healing process can vary from one patient to the next, and it is normal to experience pain just after the surgery. However, this should not last longer than a few days. Patients may also experience:
- Vaginal bleeding lasting for about two weeks post-surgery.
- Tenderness in the abdominal area, lasting one to three days after surgery.
- Shoulder pain lasting up to two days after surgery.
The symptoms of endometriosis may return within one year of surgery. The rate of recurrence is usually greater than more time goes by.
